What?
Placenta encapsulation is the process of drying and grinding your placenta to put into capsules. This is very popular with mothers, and is reported to help with recovery as well as help to avoid postpartum depression and build milk supply. The fee for encapsulation is $250.
Why?
In animal studies, it has been proven that the oral ingestion of species-specific placenta has a direct effect on hormone levels in the postpartum period. It has also been determined that the active ingredients in the placenta are effective only when taken by mouth, and that consuming placenta from another species will not reproduce benificial effect. It is theorized that encapsulated placenta may help our bodies to combat our shifting hormones by re-introducing hormones that are found in the placenta itself, or by other, less understood, means.
Hormones are amazing and complicated substances. During pregnancy many hormones are found in the body in much higher quantities than is found in non-pregnant women. These hormones work in an interconnected way within our bodies. At the time of birth, many of these hormones are dramatically withdrawn from our system, and can cause our mood regulation to go haywire.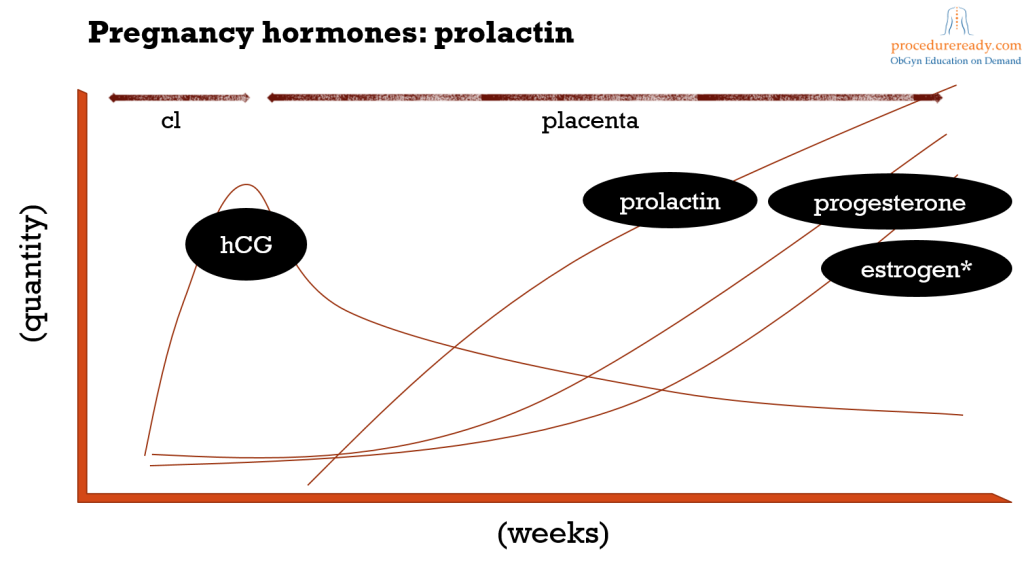
Some of these hormones and their actions are:
- Estrogen rises during pregnancy due to production of the placenta and the fetal liver. The high estrogen levels stimulate the body to produce thyroid hormone-binding globulin, which raises levels of bound thyroid hormones. This rise in bound thyroid hormones stimulates, in turn, an increase in thyroid-stimulating hormone and, therefore, an increase in unbound thyroid hormones to maintain proper percentages.
- Progesterone, also produced by the placenta, raises to levels many times that found in non-pregnant women and, also dramatically declines upon the delivery of the placenta.
- Cortisol, peaks at the end of pregnancy due to placental production of corticotrophin releasing hormone, and quickly falls at delivery.
- Corticotrophin Releasing Hormone is secreted by the placenta and rises to three times the pre-pregnant amount. CRH is usually secreted, in response to stress, by the hypothalamus and causes a hormonal chain reaction which increase the stress hormone cortisol, but during pregnancy levels rise WITHOUT causing a corresponding release of cortisol.
- Prolactin rises significantly during pregnancy, and drops dramatically unless a woman nurses her baby (although levels will return to normal eventually, even in nursing mothers).
- Oxytocin, from the pituitary, actually rises dramatically at deliver, and is important in stimulating uterine contractions, in breastfeeding, and is thought to be the “maternal instinct” hormone.
- Vasopressin, another pituitary hormone, which regulates blood pressure, has been noted in depressed levels in the urine of postpartum women.
While none of these hormones has been implicitly indicted as a cause for postpartum depression, several interesting studies have raised questions about their possible roles.
- Studies have shown that estrogen therapy does aid in postpartum depression, even though no test has yet determined why that is.
- It has also been shown that postpartum women have double the incidence of thyroid dysfunction as compared to the general population. This dysfunction is known to carry a high incidence of depression that resolves once the thyroid issue is addressed. It is reasonable to wonder, then, if even sub-clinical levels of thyroid imbalance might also exacerbate PPD.
- Serotonin may play a role in PPD, as one type of estrogen may act as a helper to its production and as an antagonist to its breakdown, so the dramatic drop in this type of estrogen that occurs at delivery may contribute to low serotonin, and therefore to PPD. Thyroid hormones also influence the levels of serotonin.
- Progesterone therapy, in one experiment, did reduce symptoms of PPD, though no scientific study has been conducted
- Prolactin levels, when studied, have produced confusing results in regard to PPD, but cannot be ruled out as significant.
- Oxytocin and Vasopressin have not been studied, and so cannot be ruled out. It is worthwhile to note that oxytocin is a chemical that is nicknamed the “trust” or “mothering” hormone, and that fluctuating levels (especially in the absence of breastfeeding) might certainly influence mood.
- Cortisol has not shown any relation to PPD; however, a study of adrenal suppression following cortisol withdrawal has indicated a possible link to PPD.
- Corticotrophin releasing hormone deficiency has been directly linked to depression. In one report, postpartum women showed low levels of CRH and the women with the lowest levels felt depressed. It is thought that the high levels of CRH in the blood stream at the end of pregnancy basically short circuits the CRH “thermostat” in the hypothalamus, and that it takes some time for the hypothalamus to start producing the CRH again.
We know that most mammals ingest the placenta after birth. There have been many attempts to explain this, but the most prevalent theory used to explain placentophagy (consuming the placenta) in mammals – that it is just an attempt to clean up the birth site and make it less inviting to predators – just doesn’t hold water. This common theory can be disproved by the exploration of three key facts. Firstly, even animals whose offspring can quickly stand and walk away from the birth site stay to finish consuming the placenta. Second, predators who are at the top of the food chain, and so have little worry of attack, consume their placentas. Finally, primates that give birth in trees do not let the placenta drop to the ground, where it would be far away from their nest site, but instead hang onto it and consume it, even though it can take over an hour to do so. It is also worth noting that animals do not attempt to remove the birth fluids from the birth site, which seems to disprove the idea that placentophagy an effort to obscure signs or smells of birth.
One more likely hypothesis is that placentophagy helps a new mother to restore the iron balance in her body. In the US, More than 1 in 10 women suffer from iron deficiency during the six-month period following childbirth. Low iron in new mothers can cause fatigue, among other symptoms. This is a serious consideration, especially because research has demonstrated a strong link between iron deficiency and postpartum fatigue, AND a strong link between postpartum fatigue and postpartum depression! In fact, one study found that postpartum fatigue, as measured on day 14 postpartum, was an effective predictor of PPD in a striking 10 out of 11 women!
Luckily, fatigue seems to be correctable with iron supplementation. One study showed that, even in the absence of clinical anemia, iron supplementation helped women with general fatigue symptoms to feel better. Anecdotally, women who ingest their encapsulated placenta also report feeling less tired. We suspect that this is partially because the placenta contains a significant percentage of the maternal iron stores. We Americans may be surprised about this, but the Chinese have used placenta to treat fatigue for many generations. As it turns out, fighting fatigue may well be fighting postpartum depression.
Milk supply is another area in which the placentophagy is proven to provide great benefit. According to the results of a Russian study, there is significant evidence that ingesting the placenta does increase milk supply in new mothers. This research shows that over 80% of women who received their placenta in the postpartum period had measurable increase in milk production. These women enjoyed more milk with no worry about harmful side effects or allergic reactions that can appear with other substances used to increase milk supply.
In summary, the existing research seems to lend credence to the benefits that are reported by the women who have had their placenta’s encapsulated. We know that, in addition to the proven lactation benefits, you might enjoy decreased fatigue and be less susceptible to postpartum depression. Basically, it will probably help, and it cannot hurt!